Tropical Medicine Research Center (TMRC) Project
Epidemiology and transmission of Leishmania donovani infections in Sri Lanka and Bhutan
Parasitic Diseases Research Unit, Department of Parasitology
Faculty of Medicine

The Tropical Medicine Research Center (TMRC) project is financially supported by the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH), USA through a TMRC Award (Grant No. U01AI136033). TMRC grants are much sought after and highly prestigious awards given every 5 years, with only Seven Centers across the world awarded such grants during the last cycle in the year 2017 (https://www.niaid.nih.gov/research/tropical-medicine-research-centers). The project was initiated in 2017 by a team at the Parasitic Disease Research Unit and is led by Professor Nadira Karunaweera, Senior Professor and Chair of Parasitology in collaboration with the University of California, Irvine, USA and the Khesar-Gyalpo University of Medical Sciences of Bhutan.
Main aims of this study include (i) understanding the occurrence, the disease process in humans, its management and the spread of leishmaniasis in Sri Lanka and Bhutan using biological, epidemiological and molecular tools, (ii) dissecting the role and properties of the vector and its environment to enable infection control in Sri Lanka and Bhutan and (iii) investigating genetic factors in Phlebotomus argentipes associated with transmission efficiency and dynamics in Sri Lanka.
The leishmaniases are a group of diseases that are considered among the least studied and most neglected of tropical diseases. Cutaneous leishmaniasis (CL) is an established disease in Sri Lanka with an outbreak situation that occurred in 2001 with a steady rise in disease incidence to date. This funding support from the NIH, USA to the University of Colombo in 2017, was a continuation of financial support that started in 2012 through an R01 Award (NIH AI099602) that sponsored the pioneering research program on leishmaniasis that Prof. Karunaweera and her team continues since the year 2001 (with the initial funding support coming from the National Science Foundation, Sri Lanka and the University of Colombo) [LINK]. The collaborations built through the TMRC award are designed to facilitate research on the cause, diagnosis, disease pathology, pathogenesis, effective disease management, prevention, control and to create and sustain in-country research capacity with strengthened international collaborations. The ongoing studies continue to provide critical information in a systematic manner, on many aspects of leishmaniasis with a special focus on diagnosis, patient management, epidemiology, vector ecology and transmission, which are desperately needed for national-level planning of leishmaniasis control and subsequent elimination both in Sri Lanka and Bhutan
COVERAGE OF THE TMRC PROJECT
Tropical Medicine Research Center Project (TMRC)
Epidemiology and transmission of Leishmania donovani infections in Sri Lanka and Bhutan
Program Director/ Principal Investigator: Professor Nadira Karunaweera
Co-Principal Investigator: Guofa zhou
Principal Investigator (Bhutan) Sithar Dorjee
- OBJECTIVE 1: To gain better insights into the occurrence, disease process in humans, its management and the spread of leishmaniasis in Sri Lanka and Bhutan using biological, epidemiological and molecular tools
Project Leads: Sri Lanka: Nilakshi Samaranayake, Hermali Silva, Nuwani Manamperi (Sri Lanka)
Research Trainees: Sithar Dorjee, Tashi Tobgay (Bhutan)- Clinical Core & Public Face of Science: Panduka Karunanayake
- Awareness programs for Medical/Paramedical /Public health officers: Nilakshi Samaranayake, Hermali Silva, Nuwani Manamperi, Sanath Senanayake
- Data and Administrative Core: Rajika Dewasurenda (Lab and data manager), Upul Senerath (Consultant)
- OBJECTIVE 2: Dissect the role and properties of vector and its environment that are important in infection transmission and control in Sri Lanka and Bhutan
Project Lead: Sanath Senanayake (Sri Lanka)
Research Trainees and Field Staff: Tenzin Wngdi (Bhutan)- Data and Administrative Core: Rajika Dewasurenda (Lab and data manager), Upul Senerath (Consultant)
- OBJECTIVE 3: To investigate genetic factors in Ph. argentipes associated with transmission efficiency and dynamics in Sri Lanka
Project Lead: Nissanka de Silva (Sri Lanka)
THE TEAM

Professor Nadira Karunaweera
Program Director, Chair and Senior Professor,
Department of Parasitology, Faculty of Medicine
University of Colombo

Dr Guofa Zhou
Co-Principal Investigator, Associate scientist
College of Health Sciences
University of Califonia – Irvine USA
Lead Investigators – Sri Lanka

Professor B.G.D.N.K De Silva
Professor, Department of Zoology
University of Sri Jayawardenepura

Professor Upul Senarath
Professor, Department of Community Medicine
Faculty of Medicine, University of Colombo

Dr Panduka Karunanayake
Senior Lecturer, Consultant Physician
Department of Clinical Medicine
Faculty of Medicine, University of Colombo

Dr Sanath Senannayake
Senior Lecturer, Department of Parasitology
Faculty of Medicine, University of Colombo

Dr Nilakshi Samaranayake
Senior Lecturer, Department of Parasitology
Faculty of Medicine, University of Colombo

Dr Nuwani Manamperi
Senior Lecturer, Department of Parasitology
Faculty of Medicine, University of Kelaniya

Dr Rajika Dewasurendra
Lab and data manager
Department of Parasitology
Faculty of Medicine, University of Colombo

Dr N. Hermali Silva
Lecturer, Department of Parasitology
Faculty of Medicine
University of Colombo
Lead Investigators - Bhutan

Dr Sithar Dorjee
Director/ Assistant Professor of Epidemiology
Khesar-Gyalpo University of Medical Sciences – Bhutan

Dr TashiTobgay
Director of Human Resource, Planning & International Relations
Khesar Gyalpo University of Medical Sciences, Bhutan

Mr Tenzin Wangdi
Medical entomologist
Vector-borne disease control program
Ministry of Health Bhutan
CASE-CONTROL STUDY
Project research assistants visited the households in selected MOH areas to collect data and blood samples from reported leishmaniasis cases and relevant controls.
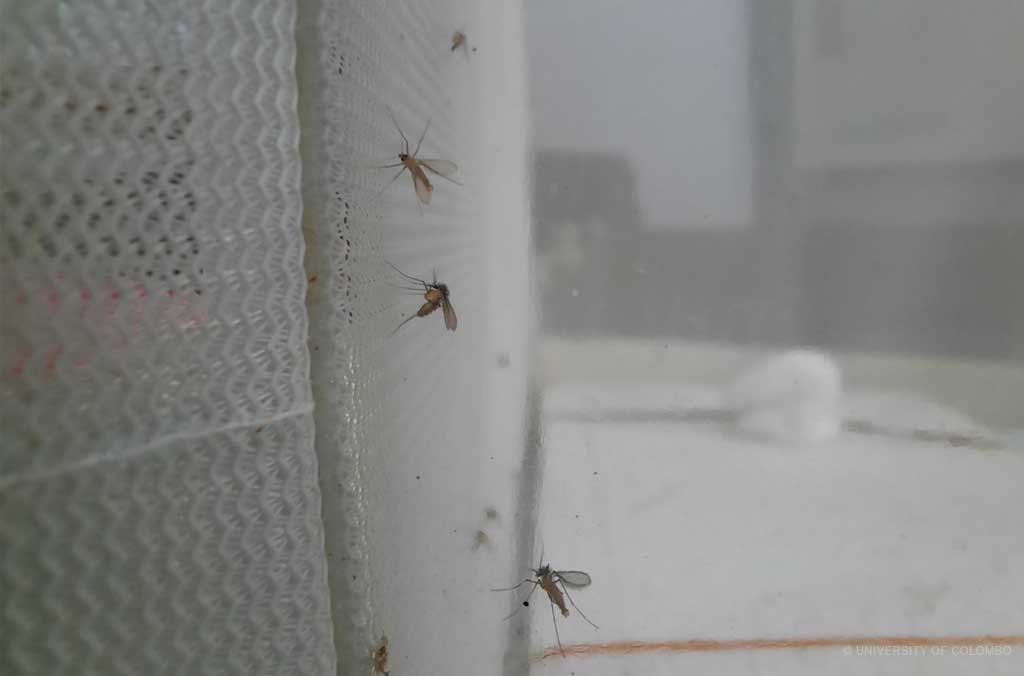
CAPTURING SANDFLIES USING CATTLE – BAITED TRAPS
STUDY OF THE GENETICS OF THE VECTOR
PUBLIC FACE OF SCIENCE AND AWARENESS PROGRAMS
SCIENTIFIC ACCOMPLISHMENTS AND PUBLICATIONS
- Siriwardana Y, Deepachandi B, Weerasinghe S, Karunaweera N, Udagedara C, Warnasuriya W, Ranawaka RR, Kahawita I. (2021). First Evidence from Sri Lanka for subphenotypic diversity within L. donovani-induced classical cutaneous leishmaniasis. BioMed Research International. 2021: Article ID 3537968. https://doi.org/10.1155/2021/3537968
- Silva H, Liyanage A, Deerasinghe T, Sumanasena B, Munidasa D, de Silva H, Weerasingha S, Fernandopulle R, Karunaweera ND. (2021).Therapeutic response to thermotherapy in cutaneous leishmaniasis treatment failures for sodium stibogluconate: A randomized controlled proof of principle clinical trial. American Journal of Tropical Medicine and Hygiene. 104(3): 945-950. https://doi.org/10.4269/ajtmh.20-0855
- Karunaweera ND et al., (2020). Spatial Epidemiologic Trends and Hotspots of Leishmaniasis, Sri Lanka, 2001–2018. Emerging Infectious Diseases. 26(1). https://doi.org/10.3201/eid2601.190971
- Pathirage DRK et al., (2020). Insecticide susceptibility of the sand fly leishmaniasis vector Phlebotomus argentipes in Sri Lanka. Parasite Vectors 13(1): 246. https://doi.org/10.1186/s13071-020-04117-y
- Pradhan A, et al., (2020). Atypical presentation of post-kala-azar dermal leishmaniasis in Bhutan. Case Reports in Dermatological Medicine 2020: Article ID 8899586, https://doi.org/10.1155/2020/8899586
- Ahuja K, et al., (2020). High Resolution Melting based method for rapid discriminatory diagnosis of co-infecting Leptomonas seymouri in Leishmania donovani-induced leishmaniasis. Parasitology International. 75: 102047. https://doi.org/10.1016/j.parint.2019.102047
- Deepachandi B et al, Quantification of soluble or insoluble fractions of Leishmania parasite proteins in micro-volume applications: a simplification to standard Lowry assay. International Journal of Analytical Chemistry. 2020: 6129132. https://doi.org/10.1155/2020/6129132
- Siriwardana Y et al., (2019). First Evidence for Two Independent and Different Leishmaniasis Transmission Foci in Sri Lanka: Recent Introduction or Long-Term Existence? Journal of Tropical Medicine https://doi.org/10.1155/2019/6475939
- Deepachandi B, et al., (2019). A highly sensitive modified nested PCR to enhance case detection in leishmaniasis. BMC Infectious Diseases 19:623. https://doi.org/10.1186/s12879-019-4180-3
- Ejazi SA et al., (2019). A multicentric evaluation of dipstick test for serodiagnosis of visceral leishmaniasis in India, Nepal, Sri Lanka, Brazil, Ethiopia and Spain. Scientific Reports. 9:9932. https://doi.org/10.1038/s41598-019-46283-9
- Siriwardana Y, et al., (2019). Leishmania donovani induced cutaneous leishmaniasis: an insight into atypical clinical variants in Sri Lanka. Journal of Tropical Medicine. https://doi.org/10.1155/2019/4538597
- Siriwardana Y, et al., (2019). Trends in recently emerged Leishmania donovani induced cutaneous leishmaniasis, Sri Lanka, first 13 years. BioMed Research International. Volume 2019, Article ID 4093603, https://doi.org/10.1155/2019/4093603
- Samarasinghe SR, et al., (2018). Genomic insights into virulence mechanisms of Leishmania donovani: evidence from an atypical strain. BMC Genomics. 28; 19(1):843. https://doi.org/10.1186/s12864-018-5271-z
- Refai W, et al., (2018). Cutaneous leishmaniasis in Sri Lanka: effect on quality of life. International Journal of Dermatology. https://doi: 10.1111/ijd.14240.
- Siriwardana YD, et al., (2018). Evidence for seroprevalence in human localized cutaneous leishmaniasis caused by L. donovani in Sri Lanka. Biomed Research International 17; 2018: 9320367. https://doi.org/10.1155/2018/9320367
- Manamperi NH, et al., (2018). Tissue impression smears as a supplementary diagnostic for histopathology for cutaneous leishmaniasis in Sri Lanka. American Journal of Tropical Medicine and Hygiene. 98(3):759-762. https://doi.org/10.4269/ajtmh.17-0748
- Kaunaweera ND, Ferreira MU. (2018). Leishmaniasis: Current challenges and prospects for elimination with special focus on the South Asian region. Parasitology. 12:1-5. doi: https://doi.org/10.1017/s0031182018000471
- Kariyawasam KKGDUL, et al., (2018). Dermotropic Leishmania donovani in Sri Lanka: Visceralizing potential in clinical and preclinical studies. Parasitology. 145(4):443-452. https://doi.org/10.1017/S003118201700169X
- Kariyawasam KKGDUL, et al., (2017). Genetic diversity of Leishmania donovani that causes cutaneous leishmaniasis in Sri Lanka: a cross sectional study with regional comparisons. BMC Infectious Diseases, 17:791. https://doi.org/10.1186/s12879-017-2883-x
- Siriwardana HVYD et al., (2017). Emergence of visceral leishmaniasis in Sri Lanka: a newly established health threat. Pathogens and Global Health, 111:6, 317-326. https://doi.org/10.1080/20477724.2017.1361564
- Manamperi NH, et al., (2017). In situ immunopathological changes in cutaneous leishmaniasis due to Leishmania donovani. Parasite Immunology; 39 (3). https://doi.org/10.1111/pim.12413
- Refai W et al., (2017). Efficacy, safety and cost-effectiveness of thermotherapy in the treatment of Leishmania donovani-induced cutaneous leishmaniasis: A randomized controlled clinical trial. American Journal of Tropical Medicine and Hygiene, 97(4):1120-1126. https://doi.org/10.4269/ajtmh.16-0879
HUMAN RESOURCE DEVELOPMENT/ TRAINING OPPORTUNITIES/ SCIENTIFIC CONFERENCES
Human resource development in the field of leishmaniasis:
PhDs completed and ongoing
- Dr. Yamuna Siriwardana (2008) (the first PhD on leishmaniasis in Sri Lanka)
Current position: Head of Department and Senior Lecturer in Parasitology, Faculty of Medicine, Colombo
Thesis title: Clinical epidemiology of cutaneous leishmaniasis in Sri Lanka and molecular identification of the parasite - Dr. Nilakshi Samaranayake (2011)
Current position: Senior Lecturer in Parasitology, Faculty of Medicine, Colombo.
A candidate gene association study of genetic susceptibility to cutaneous leishmaniasis in Sri Lanka - Udeshika Kariyawasam (2018)
Current position: Postdoctoral Scientist, Oklahoma State University, USA.
Thesis title: Phenotypic and genetic characteristics of Leishnania donovani that cause cutaneous Ieishmaniasis in Sri Lanka - Nuwani H. Manamperi (2018)
Current position: Senior Lecturer in Parasitology, Faculty of Medicine, University of Kelaniya.
Thesis title: Host factors in the pathogenesis of cutaneous leishmaniasis due to Leishmania donovani in Sri Lanka. - Sanath Senanayake (Ongoing Ph. D. project)
Current position: Senior Lecturer in Parasitology, Faculty of Medicine, Colombo
Project Title: Studies on vector of leishmaniasis and its transmission - Hermali Silva (Ongoing Ph. D. project)
Current position: Lecturer in Parasitology, Faculty of Medicine, Colombo
Project title: Parasite determinants that influence the treatment outcome in cutaneous leishmaniasis in Sri Lanka - Dulani Pathirage (Ongoing Ph. D. project)
Current position: Research Assistant
Project title: Phlebotomus argentipes, the vector of leishmaniasis in Sri Lanka; mechanisms and propagation of insecticide resistance. - Hasna Riyal (Ongoing Ph. D. project)
Current position: Research Assistant
Project title: Host innate immune mechanisms, parasite phenotypes and genetics in pathogenesis of cutaneous leishmaniasis in Sri Lanka.
Research grant awarded as an off-shoot of the NIH parent project: CRDF Global, National Institute of Health. Ref. No. 28862 (2019-2021)
Title: Interdisciplinary Study of Factors Related to Treatment Outcome of Sri Lankan Cutaneous Leishmaniasis” was selected to receive the U.S.-Japan Cooperative Medical Sciences Program Collaborative Award, 2019
Principal Investigator: Dr. Hermali Silva; Co-Principal Investigator: Prof. N.D. Karunaweera
Amount: USD 45,000 (LKR 8.1 million)
MD Training
- Sanath Senanayake (2007)
Degree: MD (Microbiology with special interest in Parasitology)
Title: Study on Phlebotomine Sandflies in selected areas of Sri Lanka
Current position: Senior Lecturer in Parasitology, Faculty of Medicine, Colombo - Wardha Refai (2016)
Degree: MD (Microbiology with special interest in Parasitology)
Title: Study of behavioural patterns in cutaneous leishmaniasis (CL) and efficacy and cost-effectiveness of a novel treatment method for CL in Sri Lanka
Current position: Consultant Parasitologist/ Entomologist, Medical Research Institute, Ministry of Healthcare, Sri Lanka. - KTGMP Kariyawasam (2016)
Degree: MD (Community Medicine)
Title: Cutaneous leishmaniasis: developing a valid and reliable instrument for community-based case detection and epidemiology in Polonnaruwa district
Current position: Consultant Community Physician, Ministry of Healthcare, Sri Lanka.
M. Phil Training
- Hiruni Wijesooriya (2020)
Title: Role of host innate cellular immune response in infections by L. donovani
Current position: Project Manager, Tobacco Observatory, Regional office, Colombo.
M.Sc. in Molecular Medicine
- Dr. GSP Ranasinghe (2012)
Dissertation title: Setting up of a serological assay for diagnosis of leishmaniasis and seroprevalence of anti-leishmania antibodies in patients whose diagnosis has been confirmed through PCR.
Current Position: Consultant, Medical Administration, Ministry of Health, Colombo. - Dr. Kalpani Kumarasiri (2020/2021): Ongoing study.
Project title: use of molecular methods to study the source of blood meal and Leishmania donovani infection in Phlebotomus argentipes sandflies from selected areas in Sri Lanka
Training Opportunities
Training opportunities for the research trainees and project research staff at prestigious international and local research institutes and universities that include: Wellcome Trust Genome Campus, Sanger Institute, Hinxton, UK; Ohio State University, USA; National Institutes of Health Research Laboratories, USA; International Centre for Genetic Engineering and Biotechnology (ICGEB), in Trieste, Italy; Institute of Molecular Medicine, New Delhi, India, Monash University Malaysia; European Molecular Biology Laboratory (EMBL), Germany; University of Kelaniya Sri Lanka and University of Peradeniya, Sri Lanka.
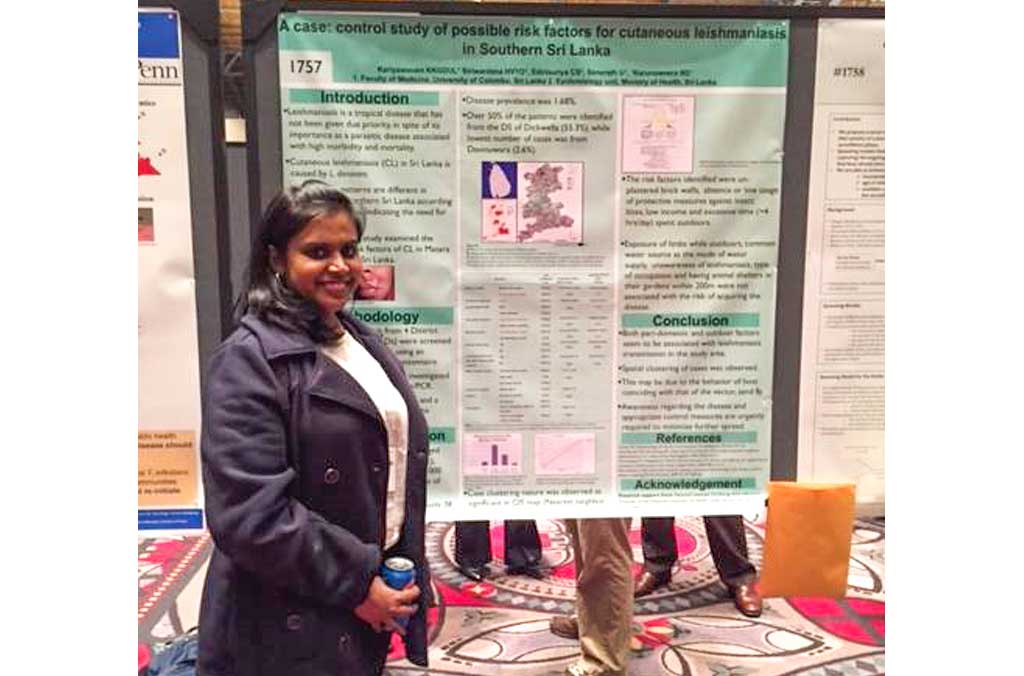
Networking and dissemination of information through scientific conferences
Research trainees present their work in international and local conferences: Annual scientific conference of the American Society for Tropical Medicine and Hygiene (ASTMH); World Congress on Leishmaniasis, International Congress on Infectious Diseases, Gordon Research Conference on Tropical Infectious Diseases, Annual Scientific Sessions of the Sri Lanka Medical Association, Sri Lanka College of Microbiologists, Sri Lanka Society for Microbiology, University Research Sessions.
INFRASTRUCTURE DEVELOPMENT
A well-equipped research laboratory was established in 2016 to facilitate lab work and research training. New equipment was purchased for the culture room, where Leishmania parasites are cultured for research. A new freezer room was established with -30ºC/ -80ºC freezers and fridges to store samples and reagents. Insectary facilities have been upgraded for rearing sandflies and office space was developed to carry out project administration and financial activities; a data room for database development and analyzing activities; a conference room for discussions and holding meetings.
IMPROVEMENT OF DISEASE AWARENESS OF THE HEALTH STAFF & GENERAL PUBLIC AND KEY OUTCOMES
Key outcomes of public health significance
- Mapping the areas with the highest burden of leishmaniasis, to enable prioritization in the implementation of control measures.
- Introduction of thermotherapy as a cost-effective option for treatment of cutaneous leishmaniasis and to better manage patients who have failed to cure with routine drugs.
- Demonstration of insecticide susceptibility patterns in sand flies from the field with implications for future chemical control.
- Introduction of diagnostics with higher sensitivity.
- Better insights into the mechanism of disease (pathogenesis) of causative parasite, L.donovani with implications for better patient management
KEY SCIENTIFIC FINDINGS OF PUBLIC HEALTH SIGNIFICANCE
PUBLICATIONS
- Karunaweera ND, Ferreira MU. (2018). Leishmaniasis: current challenges and prospects for elimination with special focus on the South Asian region. Parasitology. 12:1-5. https://doi.org/10.1017/S0031182018000471
- Karunaweera ND (2016). Leishmaniasis: Path towards elimination from the Indian subcontinent. Tropical Parasitology. 6(1): 2-4.
- Siriwardana HVYD, Chandrawansa PH, Sirimanna G, Karunaweera ND (2012). Leishmaniasis in Sri Lanka: a decade old story (2002-2012). Sri Lanka Journal of Infectious Diseases, 2(2): 2-12. http://www.sljol.info/index.php/SLJID/issue/view/425
- Karunaweera ND (2009). Leishmania donovani causing cutaneous leishmaniasis in Sri Lanka: A wolf in sheep’s clothing? Trends in Parasitology, 25(10):458-463.
- Karunaweera ND, Rajapaksa U. (2009). Is Leishmaniasis in Sri Lanka benign and be ignored? Journal of Vector Borne Diseases, 46, 13-17.
- Karunaweera ND. Leishmaniasis: a newly established parasitic disease in Sri Lanka. (2008). Journal of the Ruhunu Clinical Society, 15:3-5.
- Siriwardana HVYD and Karunaweera ND. Leishmaniasis in Sri Lanka. (2005). Asian Parasitology. 4:257-261.
- Kothalawala HS, Karunaweera ND. (2016). Loop-mediated isothermal amplification assay as a sensitive diagnostic tool for Leishmania donovani infections in Sri Lanka. Ceylon Medical Journal 61: 68-70. http://doi.org/10.4038/cmj.v61i2.8286
- Samaranayake N, Fernando SD, Neththikumara NF, Rodrigo C, Karunaweera ND, Dissanayake VHW. (2016). Association of HLA class I and II genes with cutaneous leishmaniasis: a case-control study from Sri Lanka and a systematic review. BMC Infectious Diseases 16:292. doi:10.1186/s12879-016-1626-8.
- Refai FW, Madarasingha NP, Fernandopulle R, Karunaweera ND. (2016). Non-responsiveness to standard treatment in cutaneous leishmaniasis: A case series from Sri Lanka. Tropical Parasitology 6:155-158. http://doi.org/10.4103/2229-5070.190835
- Kariyawasam KKGDUL, Siriwardana HVYD, Edirisuriya CS, Senerath U, Karunaweera ND. (2015). Characterization of cutaneous leishmaniasis in Matara district, Southern Sri Lanka: Evidence for case clustering. Pathogens and Global Health. http://dx.doi.org.ezp-prod1.hul.harvard.edu/10.1179/2047773215Y.0000000032
- Senanayake SASC, Abeyewickrema W, Dotson E, Karunaweera ND. (2015). Characteristics of phlebotomine sandflies in selected areas in Sri Lanka. Southeast Asian Journal of Tropical Medicine and Public Health. 46(6): 994-1004.
- Siriwardana HVYD, Senerath U, Chandrawansa PH, Karunaweera ND. (2015). Use of a clinical scoring system for enhanced case detection of cutaneous leishmaniasis in Sri Lanka. Pathogens and Global Health, 109 (4):174-183.
- Siriwardana HVYD, Thalagala N, Karuanweera ND. (2010). Clinical and epidemiological studies on the cutaneous leishmaniasis caused by Leishmania (Leishmania) donovani in Sri Lanka. Annals of Tropical Medicine & Parasitology, 104(3):213–223.
- Rathnayake D, Ranawake RR, Sirimanna G, Siriwardhane Y, Karunaweera ND, De Silva R. (2010). Co-infection of mucosal leishmaniasis and extra pulmonary tuberculosis in a patient with inherent immune deficiency. International Journal of Dermatology, 49(5):549-551.
- Ihalamulla RL, Rajapaksa US, Siriwardena HVYD, Chance M, Karunaweera ND. (2009). A simple, cost-effective method for isolation and transportation of Leishmania parasites. Ceylon Medical Journal. 54(2):46-47.
- Ihalamulla RL, Siriwardana HVYD, Karunaweera ND. (2008). Efficacies of RPMI 1640 and M 199 media in the isolation of Leishmania from cutaneous lesions. Annals of Tropical Medicine and Parasitology, 102(2):173-175.
- Siriwardana HVYD, Noyes H, Beeching N, Chance ML, Karunaweera ND, Bates PA. (2007). L.donovani and cutaneous leishmaniasis, Sri Lanka. Emerging Infectious Diseases, 13(3):476-478.
- Rajapaksa US, Ihalamulla RL, Udagedera C, Karunaweera ND. (2007). Cutaneous leishmaniasis in southern Sri Lanka. Transactions of the Royal Society of Tropical Medicine and Hygiene, 101(8):799-803.
- Ihalamulla RL, Rajapaksa U, Karunaweera ND. (2006). Micro culture for the isolation of Leishmania, modified to increase efficacy: a follow-up to a previous study. Annals of Tropical Medicine and Parasitology, 100(1):87-9.
- Ihalamulla RL, Rajapaksa U, Karunaweera ND. (2005). Micro culture for the isolation of Leishmania parasites from cutaneous lesions — Sri Lankan experience. Annals of Tropical Medicine and Parasitology, 99(6):571-5.
- Rajapksa US, Ihalamulla RL, Karunaweera ND. (2005). First report of mucosal tissue localisation of leishmaniasis in Sri Lanka. Ceylon Medical Journal, 50(2):90-1.
- Karunaweera ND, Liyanage CPG, Ihalamulla RL. (2004). A simple device to maintain in vitro cultures of Leishmania in tropical countries. Transactions of the Royal Society of Tropical Medicine and Hygiene 98(5):315-317.
- Karunaweera ND, Pratlong F, Siriwardane HVYD, Ihalamulla RL, Dedet JP (2003). Sri Lankan cutaneous leishmaniasis is caused by Leishmania donovani zymodeme MON-37. Transactions of the Royal Society of Tropical Medicine and Hygiene, 97(4):380-381.
- Siriwardana HVYD, Udagedara C, Karunaweera ND. Clinical features, risk factors and efficacy of cryotherapy in cutaneous leishmaniasis in Sri Lanka. (2003). The Ceylon Medical Journal, 48(1):10-12.
- Ihalamulla RL, Siriwardane HVYD, Gamage S, Perera AJ, Karunaweera ND (2002). First successful in vitro culture of autochthonous leishmaniasis cases in Sri Lanka. The Ceylon Medical Journal, 47(2):58.
- GENETIC DIVERSITY AND POPULATION STRUCTURE OF PHLEBOTOMUS ARGENTIPES, THE VECTOR OF LEISHMANIASIS IN SRI LANKA (2021)
DR Pathirage, TC Weeraratne, SHP Karunaratne, ND Karunaweera
AMERICAN JOURNAL OF TROPICAL MEDICINE AND HYGIENE 105 (5), 173-173 - IN HOUSE ENZYME LINKED IMMUNOSORBENT ASSAY (ELISA) AS A SENSITIVE DIAGNOSTIC TOOL OF CUTANEOUS LEISHMANIASIS CAUSED BY LEISHMANIA DONOVANI (2021)
HSB Piyasiri, TN Samaranayake, NH Silva, N Manamperi
AMERICAN JOURNAL OF TROPICAL MEDICINE AND HYGIENE 105 (5), 146-146 - UTILITY OF SKIN BIOPSIES IN DIAGNOSIS AND PROGNOSIS OF CUTANEOUS LEISHMANIASIS (2021)
H Riyal, N Samaranayake, P Amarathunga, D Munidasa, N Karunaweera
AMERICAN JOURNAL OF TROPICAL MEDICINE AND HYGIENE 105 (5), 122-122 - EMERGING ENTOMOLOGICAL EVIDENCE OF INCREASED CUTANEOUS LEISHMANIASIS BURDEN IN SRI LANKA (2021)
RWC Kumarasiri, S Senanayaka, DS Shantha, B De Silva
AMERICAN JOURNAL OF TROPICAL MEDICINE AND HYGIENE 105 (5), 155-155 - ENVIRONMENTAL AND CLIMATIC DETERMINANTS OF LEISHMANIASIS RISK IN SRI LANKA: HISTORICAL VERSUS CONTEMPORARY CLIMATIC FACTORS AND LOCALIZED SEASONALITY (2021)
G Zhou, ND Karunaweera
AMERICAN JOURNAL OF TROPICAL MEDICINE AND HYGIENE 105 (5), 145-145 - PUBLIC AWARENESS ON DISEASE AND TRANSMISSION OF LEISHMANIASIS: A NATIONWIDE SURVEY IN SRI LANKALEISHMANIASIS: A NATION-WIDE SURVEY IN SRI LANKA (2021)
R Dewasurendra, N Samaranayake, H Silva, N Manamperi
AMERICAN JOURNAL OF TROPICAL MEDICINE AND HYGIENE 105 (5), 399-399 - Parasite load and its association with disease outcome in cutaneous leishmaniasis in Sri Lanka (2021)
FH Riyal, TN Samaranayake, J Ganeshalingam, AAH Priyani
Sri Lankan Journal of Infectious Diseases 11 - Knowledge, attitude and practices related to leishmaniasis among healthcare workers in an endemic area in southern Sri Lanka (2021)
HSB Piyasiri, TN Samaranayake, P Priyadarshana, GAS Hasinthara,
Sri Lankan Journal of Infectious Diseases 11 - Assessment of knowledge and perceptions in leishmaniasis: an island-wide study in Sri Lanka (2022)
R Dewasurendra, H Silva, N Samaranayake, N Manamperi
PLoS Negl Trop Dis 16 (10), e0010821 - ELISA based evaluation of antibody response to Leishmania in a region endemic for cutaneous leishmaniasis (2022)
SB Piyasiri, TN Samaranayake, H Silva, NH Manamperi, K ND
Parasite Immunology, e12940 - Treatment of cutaneous leishmaniasis; with insights into species-specific responses – A Narrative Review (2022)
H Silva, K Rajamanthri, K ND
Journal of Infectious Diseases and Therapy 11 (2), 695-711 - First evidence of experimental genetic hybridization between cutaneous and visceral strains of Leishmania donovani within its natural vector Phlebotomus argentipes (2023)
H Riyal, TR Ferreira, A Paun, K Ghosh, N Samaranayake, DL Sacks
Acta Tropica 245, 106979 - Unfolded Protein Response (UPR) Pathway in cutaneous leishmaniasis: A review (2023)
N Karunaweera, NM Edirisinghe, N Manamperi, VS Wanasinghe - Cytokine and phenotypic cell profiles in human cutaneous leishmaniasis caused by Leishmania donovani (2023)
H Wijesooriya, N Samaranayake, ND Karunaweera
Plos one 18 (1), e0270722
PROMOTING AWARENESS
Promoting awareness on ‘local transmission of leishmaniasis in Sri Lanka’ among local policymakers, scientists, professionals and the international community and development of a ‘national framework for its prevention and control
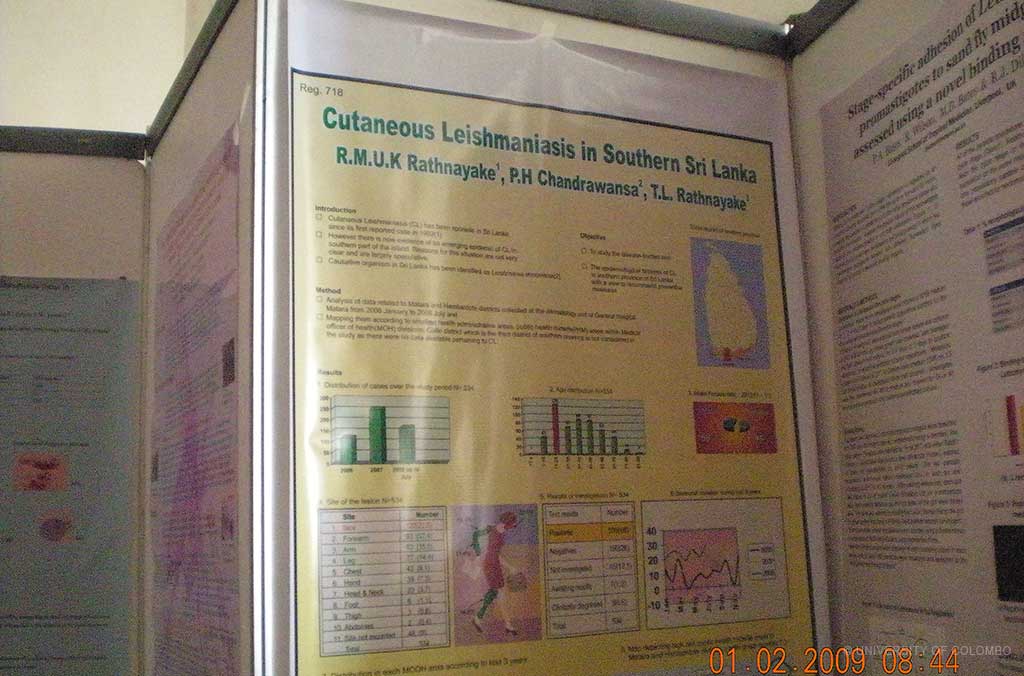
- 2009 February (Colombo): International Colloquium on Leishmaniasis in Sri Lanka, organized by the University of Colombo (Sponsored by National Science Foundation, TEHDA. Featuring invited experts from India, Brazil and France. Attended by stakeholders from all 9 provinces. Included lectures, poster presentations of research, and development of a national action plan for prevention and control of cutaneous leishmaniasis.
- 2013 March (Colombo): 2nd International Colloquium on Leishmaniasis in Sri Lanka, organized by the University of Colombo. Sponsored by NSF. Features invited experts from India. Attended by stakeholders from all relevant sectors. Updated the national action plan and also included visceral leishmaniasis.
FUNDING SUPPORT
- University of Colombo AP/3/2011/CG/01
- National Science Foundation RG/SIDA/2002/M/01; RG/SIDA/2003/M/01; RG/2005/HS/07; RG/2011/HS/13
- National Institute of Health USA R01AI099602: Significant as the 1st NIH grant awarded to a Sri Lankan University
RESEARCH ASSISTANTS
THE CASE-CONTROL STUDY – FIELD TEAM
Ms Ruksala Ranatunga (2018-2019)

Ms Sacheebhanu Piyasiri (2018- To Date)

Mr Nishanthan Chandrasekharan (2018-2019)

Mr Dasun Madushan (2018)

Mr Chathura Priyadharshana (2019)

Mr Sandeep Hasinthara (2019)

Ms Gishani Parameswaran (2020)

VECTOR AND ITS ENVIRONMENT
Mr Raushan Siraj (2018 - 2020)

Mr M. Ariyapala (Field Assistant) (2019 - To Date)

Mr Sunil Shantha - Entomological Assistant (2019- Todate)

Mr Amila Suraj (2021 - To Date)

IMMUNOLOGY/ GENETICS
Ms Tharushi Alles (2019 – 2020)

Ms Isurika Weerasinghe (2021 - To Date)

Ms Vishmi Wanasinghe (2021 - To Date)

Ms Sumudu Sarasija (2021 - To Date)

POST-DOCTORAL SCIENTISTS
Dr Pamoda Jayatunga (2021 - To Date)

Dr Akash Fernando (2019)

VECTOR GENETICS
Dr Kalpani Kumarasiri (2020) – MD trainee (Molecular Medicine)

Ms Nadeesha Senarath (2020 - To Date)

Ms Shriyani Ranatunga (2021 - To Date)

DRUG RESISTANCE STUDIES
Mr Kasun Madusanka (2020 - To Date)

BIOINFORMATICS
Ms Sumudu Samarasinghe (2018 - To Date)

RA – PUBLIC FACE OF SCIENCE
Mr Chamara Sihan (2021 - To Date)

PHD/ MPHIL STUDENTS
Dr Udeshika Kariyawasam (2013 - 2018)

Ms Dulani pathirage (2018 - To Date)

Ms Hasna Riyal (2018 - To Date)

Ms Hiruni Wijesooriya (2017 – 2020)

ADMINISTRATIVE AND FINANCE STAFF
Ms Letitia de Silva (2018)

Ms Wajira Peiris (2018-2019)

Ms Kanchana Sewwandi (2019-2020)

Ms Niluka Perera (2020)

Dr Achala Ranasinghe (2020 - To Date)

Ms Nimesha Madumali - Finance (2018)

Ms Thilini Madhushya - Finance (2018-2019)

Ms T. Sadhusha - Finance (2020 - To Date)

Ms Maheshika Gunarathne - Data entry (2019 - To Date)